Jun 3, 2021 | Insights
How can MedRisk services help streamline treatment for neck injury patients? Manager of Clinical Services Suzanne Sadusky, PT, DPT, shares the important role her team plays in injured worker recovery.
This blog is part 3 of a 3-part series titled “Neck Injuries in Workers’ Comp: Managing Pain and Controlling Cost.”
Neck injury can be a complex treatment area for physical medicine clinicians. From headaches to nerve pain, the symptoms of neck injury can be wide-ranging, which can increase the cost of diagnosis and treatment if not managed appropriately.
MedRisk aims to simplify the pathway to recovery for injured workers, including those being treated for neck injury. We sat down with Suzanne Sadusky, PT, DPT, MedRisk’s Manager of Clinical Services, to discuss the journey of a neck injury referral and how MedRisk supports streamlined, cost-effective treatment every step of the way.
1. Pre-Treatment Services
As soon as a referral is made, MedRisk gets to work in matching the patient with an appropriate provider based on specialty, location, and availability – within an average of 4 hours. This helps patients be seen for an initial evaluation within 2.6 days of referral. First, the patient may consult with one of MedRisk’s on-staff physical therapists prior to treatment. During this dialogue, the PT can identify things that could impact recovery, such as prior surgeries, existing ailments, and psychosocial factors such as depression or anxiety. Notes from the consult are delivered to stakeholders in a comprehensive report, which allows these insights to be considered in developing an optimal treatment plan. In addition, the PT uses the consultation to educate the patient on the treatment process, set expectations for recovery and encourage patient participation and compliance.
“We try to alleviate any anxiety about starting therapy and answer their questions,” Sadusky said. “We are not the treating therapist and we are not the insurance carrier. We are a third party, which puts us in a unique position.”
2. Clinical Oversight
As the first company to introduce evidence-based guidelines for managed physical medicine, MedRisk is committed to keeping treatment guidelines up to date. The company’s proprietary guidelines, which are categorized by body part, are assigned to every case that opens at MedRisk, and they help set expectations for the number of visits and the amount of time that is expected for recovery. The guidelines were developed by and are maintained by MedRisk’s International Scientific Advisory Board (ISAB), an elite panel of world-renowned specialists in physical medicine and workers’ compensation who oversee all clinical aspects of MedRisk’s medical management programs. The group meets regularly to review current scientific literature and new treatment protocols and vet MedRisk’s guidelines, which are specific to physical therapy and workers’ compensation.
“The guidelines go a long way in keeping treatment on track. However, there will always be instances when patients do not progress as expected,” Sadusky said. In these cases, Sadusky’s team is called upon to do a clinical review. During this process, the team reviews the case documentation and reaches out to the treating therapist to discuss whether additional therapy is necessary. With these insights in hand, MedRisk is then able to provide recommendations to adjusters on how to optimize treatment moving forward.
3. Telerehabilitation
Telerehabilitation has become a more standard component of treatment throughout the pandemic, and according to Sadusky, the benefits will hold up well into the future.
“During COVID, it often wasn’t always safe or possible to be in the clinic, and it really showed how telerehab can support continuity of care,” she said. The option of receiving PT services from home can help patients avoid gaps in treatment, maintain steady progress, and control their symptoms in the expected timeframe. In the case of neck injury, patients may receive equipment, including TheraBands, an exercise ball, and weights, with instruction for self-management and advanced strength exercises through a virtual PT appointment. This allows patients to avoid common pitfalls that could have derailed in-person treatment, extended the duration of the claim, and potentially delayed return to work.
Conclusion
What presents as neck pain can often be more complex than meets the eye, as the injury can sometimes involve the shoulder or spine. When treating a clinically complex injury, it’s important that treatment plans are both patient-centered and streamlined. Through MedRisk’s managed physical medicine services – communication with patients and stakeholders, clinical oversight, and telerehabilitation – a more predictable and cost-effective path to recovery can be achieved.
About Suzanne Sadusky, PT, DPT
Suzanne is a licensed physical therapist. She has worked at MedRisk for over 6 years and is currently the Manager of MedRisk’s Clinical Services team. Her team is responsible for performing clinical reviews and providing documented recommendations based on use of appropriate clinical guidelines. Suzanne holds a Doctor of Physical Therapy degree from Boston University and a Bachelor’s in Health Studies degree also from Boston University. Prior to joining MedRisk, Suzanne worked in a variety of settings as a physical therapist. These include outpatient orthopedics and workers’ compensation, acute care, and acute inpatient rehabilitation, as well as independent living and skilled nursing facilities. She has also been involved in facilitating online learning through Boston University’s transitional DPT program.

May 5, 2021 | Insights
What are the unique challenges faced by neck injury patients, and how can self-management strategies help them in the recovery process? Donald Murphy, DC, FRCC, weighs in.
This blog is part 2 of a 3-part series titled “Neck Injuries in Workers’ Comp: Managing Pain and Controlling Cost.”
When we think of musculoskeletal problems in workers’ comp, the first thing that comes to mind is low back pain. And with 37% of global low back pain cases believed to be work-related, this is rightfully a primary focus for the industry. But what many do not realize is that neck pain is a common issue faced not only by injured workers but the population at large. In fact, back pain and neck pain are the leading causes of years lived with disability in most countries and age groups.
We recently sat down with MedRisk International Scientific Advisory Board (ISAB) member Donald Murphy, DC, FRCC, to understand the unique challenges of treating neck pain, how therapy has evolved over the years, and strategies for effective return to work for neck injury patients.
Treatment Challenges
Getting injured on the job can be a traumatic experience. Whether it’s the effect of a fall, an accident or poor ergonomics, pain is perceived as something out of our control – and according to Dr. Murphy, this is particularly the case with neck pain.
“Neck pain is different from knee or wrist pain. The perception is that neck pain must be the result of a spine problem, and if it involves the spine, it must be a catastrophic situation,” he said.
There is a misconception that because the spine is a complex system it must be delicate and vulnerable. In actuality, the spine is one of the most protected parts of the entire body, shielded by thick ligaments and muscles. Neck pain can involve the spine, but whether a nerve root, disc, or joint is to blame, according to Dr. Murphy, educating the patient about the nature of their injury is the first step in deescalating the urge to catastrophize. The next step is getting the patient involved in their own recovery. While some passive modalities, such as manual therapy, may be a useful component of the treatment plan, he says a more active approach to treatment is essential.
The rise of telerehabilitation during the pandemic helped promote self-management strategies among injured workers. While in-person therapy is sometimes necessary and often preferred, delivering therapy virtually inherently involves instructing patients on how to help themselves. A physical therapist can demonstrate a particular neck stretch over the screen to help the patient increase mobility.
“It’s important to help the patient take an active role in their own rehabilitation. I may need to use my hands to help the situation, but the patient needs to feel empowered. I don’t want a machine to be the hero in this story. I don’t even want to be the hero in this story. I want it to be the patient,” Dr. Murphy said.
Returning to Work
It’s clear that empowering the patient is an important component of neck pain treatment, but Dr. Murphy emphasizes that this philosophy must be carried through the patient’s return to work and beyond. The likelihood of chronic pain following neck injury is often dependent on the nature of the injury; however, whether the initial cause was whiplash or ergonomics, he says it’s important to set expectations around the long-term pain experience.
“A lot of patients have a fear around returning to work. They think they shouldn’t go back until they feel 100% like they did pre-injury, or they believe going back to the same environment could lead them to hurting themselves again,” Dr. Murphy said.
He suggests talking through this fear and positioning returning to work as a natural next step in the therapy process. Getting back to normal activity, even if it triggers some level of pain, can help the process resolve as quickly and completely as possible, whereas avoiding activity can actually delay recovery. By providing patients with long-term self-management strategies and exercises that can be performed at home or on the job, they will feel better equipped to manage hurdles along the way.
“Plant that seed early,” Dr. Murphy said. “Set the expectation that the patient may feel some pain when they get back to work, but that resuming normal activity is the goal. Help them gain confidence in their ability to get their life back and provide the necessary self-management strategies to do so. With this, their pain experience often transforms.”
About Donald Murphy, DC, FRCC
In addition to serving on MedRisk’s ISAB since December 2008, Dr. Murphy is Clinical Assistant Professor at the Warren Alpert Medical School of Brown University. He is also Adjunct Assistant Professor in the Physical Therapy Department at the University of Pittsburgh, where he co-leads the Primary Spine Practitioner certificate course. He has also helped implement and direct high value spine pathways in several states through Spine Care Partners.
He has been on the Expert Panel for several spine care guidelines, including those of the American College of Environmental and Occupational Medicine, American College of Physicians and the American Pain Society. Dr. Murphy has published dozens of papers in the peer-reviewed spine literature as well as three books on back and neck pain.
Mar 5, 2021 | Insights
Injuries involving the neck are among the costliest workers’ comp claims. What are the causes, and what role does physical medicine play in recovery?
This blog is part 1 of a two-part series titled “Neck Injuries in Workers’ Comp: Managing Pain and Controlling Cost.”
As many businesses have shifted to working from home throughout the pandemic, the effect of long hours spent at a poorly designed workspace has been felt by many Americans. But poor ergonomics is just one of the many causes of neck pain among today’s workforce. In fact, injuries involving the neck are the third most costly lost-time workers’ compensation claim, behind injuries involving the head/central nervous system and multiple body parts, averaging $61,510 per claim, according to the National Council on Compensation Insurance (NCCI).
Why are neck injuries such an important focus for workers’ compensation? In this blog, we take a closer look at the nature of neck injury, methods of treatments, and the important role played by physical therapists and chiropractors in recovery.
What Causes Neck Pain?
While a claim may carry a diagnostic code for neck injury, there are often other body parts involved. Because the neck supports the weight of the head, it is particularly vulnerable to injury. Unsurprisingly, hours hunched over a computer, smartphone or book can lead to muscle strain and neck pain. However, even something as seemingly unrelated as grinding your teeth can cause neck pain and restrict motion. Additionally, if a herniated disk or bone spur is present on the vertebrae of your neck, it can put pressure on the nerves branching out from the spinal cord, leading to nerve compression and amplifying neck pain. Neck injury is also a common effect of whiplash injury in accidents such as rear-end auto collisions, which can cause the head to be jerked back and forth, straining the soft tissues of the neck. All of these triggers have the potential to have a more significant impact as we age, as neck joints wear down over time.
Diagnosing and Treating Neck Pain
In order to diagnose neck injury, a physical exam is used to assess neck function – that is, a patient’s ability to move their head forward, backward, and side-to-side – as well as symptoms such as tenderness, numbness, and muscle weakness. In some cases, imaging tests such as CT scans, x-rays or MRIs may be ordered to investigate the root cause of injury.
Once a diagnosis is made, neck injury treatment is often put in the hands of a physical therapist (PT). Among the many benefits of a more conservative approach to neck pain treatment is the reduced likelihood of opioid prescription. One study found that initially consulting with a non-pharmacological provider such as a PT can decrease opioid exposure in the year following diagnosis. PTs and chiropractors help injured workers manage neck pain and regain neck function by normalizing alignment, teaching exercises to correct muscle flexibility and strengthen deficits, and educating them on proper posture and self-care. Early on, heat, ice, and electrical stimulation may be applied along with traction, using weights and pulleys to stretch the neck – an approach often used to address nerve root irritation. In certain instances, treatment may go beyond conservative care measures to include injections of corticosteroids or numbing medications such as lidocaine to relieve neck pain; however, surgery is rarely needed.
Conclusion
As a common and costly problem among injured workers, neck injury has been a longtime focus for MedRisk. How has treatment in this area changed over the years, and where is it headed? In the remaining blog in this series, we will learn more about the nuances of neck pain treatment from MedRisk’s International Scientific Advisory Board member Dr. Donald Murphy, DC, FRCC, and explore the unique ways a managed physical medicine program can support recovery from neck injury.
Nov 4, 2020 | Insights
A closer look at how MedRisk technologies and workflows help ensure delayed processes don’t lead to delayed recoveries.
There is no doubt that physical therapy can be instrumental in getting a workers’ compensation patient back on their feet. But what happens when external factors like a shortage of providers or scheduling problems delay the start of treatment?
According to the Workers’ Compensation Research Institute’s latest research, timing is everything – or at least something the industry can’t afford to ignore. Its study, titled “The Timing of Physical Therapy for Low Back Pain: Does It Matter for Workers’ Compensation?” found that PT within 14 days of injury is likely to be beneficial and to be associated with lower utilization of medical services, lower overall medical costs and shorter temporary disability duration.
On top of this, a reduction in diagnostic tests, opioid prescriptions, pain management injections, and lumbar surgeries ultimately lead to faster return to work and lower total costs of claims. The benefits of early PT in workers’ compensation are clear.
So, how can we help ensure injured worker treatment begins stat? Here are three ways MedRisk facilitates early PT for your injured workers.
1. A Robust Provider Network
A lack of provider availability can be a big hurdle to timely treatment. One week, a patient may need a carpal tunnel specialist in a rural area while the next case requires an aqua specialist in an overbooked urban district. MedRisk’s large nationwide network has a range of PT providers – both in terms of geography and specialty. When other, smaller networks cannot meet case requirements or do not have a provider close to the patient’s home or workplace, cold calls need to be made to recruit a PT willing to take a given case. That can add days or even weeks to the process. Instead, our patient advocates schedule a patient with a provider based on their location and treatment needs within 4 hours. This helps patients be seen for an initial evaluation within 2.6 days of referral on average.
2. Technology-Backed Workflows
As described above, having a large network – and one with specialists – is integral to fulfilling a case request. But when it comes to finding the right provider at the right time, there’s more to it than having a large rolodex of names to choose from.
MedRisk’s technology ensures that a patient is matched to the most appropriate provider based on their unique needs, using criteria that go well beyond demographics and cost. Our selection process is data-driven: on the patient side, by injury type, chronicity and complexity, and on the provider side, outcomes by injury type, compliance with evidence-based guidelines, patient satisfaction and more.
Our advanced technology rapidly sifts through all of that data to present the patient advocate and the patient with a near-instant selection of the local best providers for his or her condition.
Accelerated time-to-treatment is further facilitated through MedRisk’s electronic data interchange (EDI) with insurers and other payer organizations. With EDI, patient and claim referral data pre-populates in our database, so that when the adjuster makes the referral, our patient advocates already have everything they need to schedule an appointment and that same critical information can be instantly faxed to the provider.
In states that require utilization review (UR) prior to PT, additional integration with the payers’ UR partner(s), keeps MedRisk and the adjuster informed at the same time. No need for time-consuming phone calls or emails verifying the results of the UR decision.
MedRisk has the technology, expertise–and most importantly–the resources to manage the heavy lifting in setting up the EDI.
Even when clients choose not to have EDI, we can help them implement fast referral functionality so they can refer a case with the click of a single key without exiting their claims system or picking up the phone.
Beyond these technologies, thoughtful workflows are critical to keeping referral and treatment processes on track and clinically sound. At MedRisk, we use evidence-based guidelines as our clinical foundation and have also developed historical data sets to help us identify trends that call for custom workflows. These proactive processes help us avoid delays in time to treatment.
3. A Commitment to Patient Advocacy
Injured workers are already facing physical challenges due to their injury. They may also be feeling anxious and fearful about their treatment and recovery.
Patients can receive a PT Consult prior to treatment with the goal of setting expectations, addressing fears and education about their injury and treatment.
In addition to their commitment to timely scheduling, MedRisk’s patient advocates text reminders and driving directions to help minimize no-shows, which could otherwise add 1-3 days to the start of treatment. All this can go a long way in encouraging a patient’s participation – and with it, a speedy recovery.
Conclusion
Service-oriented programs can help facilitate the timeliness of PT treatment, but at the end of the day, early PT begins with a timely referral. MedRisk has the know-how to integrate your systems to receive cases automatically – and the clinical expertise and network coverage to give them the appropriate, timely treatment they deserve.

Aug 13, 2020 | Insights
As companies establish a “new normal” for their operations, will injured worker treatment also get back on track?
As social distancing guidelines are lifted and communities around the country begin to reopen, employers are readying their workplaces for employees to return to work. However, there is one faction of the workforce for which the wait has felt particularly long, and that’s workers who have been hurt on the job before COVID-19.
In March, while the country hunkered down to “flatten the curve” of coronavirus cases in hospitals, healthcare systems braced for a potential influx of COVID-19 patients by suspending non-emergency surgical procedures, as recommended by the American College of Surgeons. As a result, researchers have estimated that 244,400 orthopedic surgeries were canceled each week during the 12-week peak disruption period in North America alone, including back surgeries, hip and knee replacements and other operations for those hurt on the job.
For many injured workers, treatment – both surgery and post-surgical physical therapy – has been put on pause. What effects has this had on physical medicine patients and providers in the workers’ comp industry, and what can we expect as the healthcare system rebounds? Let’s take a closer look.
Postponement of Elective Surgeries and Its Impact on PT
How much backlog will the healthcare system be facing as hospital operations resume?
According to an analysis from Strata Decision Technology, over a two-week period in March and April 2020, patient encounters in a hospital setting fell 54.5% when comparing it to the same period a year prior. And no specialty was immune – this trend was seen across all services lines, in every region. Primary knee replacements fell 99%, lumbar/thoracic spinal fusions declined 81% and primary hip replacement procedures fell 79%. Researchers predict that if countries increase their normal surgical volume by 20 percent post-pandemic, it would take a median 45 weeks to clear the backlog of operations.
The CDC categorized physical therapy as an essential service during the pandemic, and many patients were able to continue treatment either in-person or via telerehabilitation. However, the cancelation of elective surgeries – and with it, expected post-surgical physical therapy treatment – and patient concerns over possible viral transmission in a clinic setting had a negative impact on PT numbers nationwide. These data indicate that both orthopedists and physical therapists can expect to be managing the backlog of postponed procedures and treatment over the next year.
Effects on Workers’ Comp
PT numbers have followed a similar trend in workers’ comp. In respect to new claims, the National Council on Compensation Insurance (NCCI) expects that due to economic and employment trends, injury frequency is likely to continue its decline in most sectors, with the exception of warehousing, where there has been a hiring surge.
Pre-COVID-19, the workers’ comp industry was seeing injury rates and frequency decline overall. MedRisk data also showed a five-year trend in declining surgical cases, from 23.5% in 2015 to 17.3% in 2019; however, the number of lost time claims with physical medicine involvement continued to increase. Will the PT and conservative care movement continue in workers’ comp moving forward?
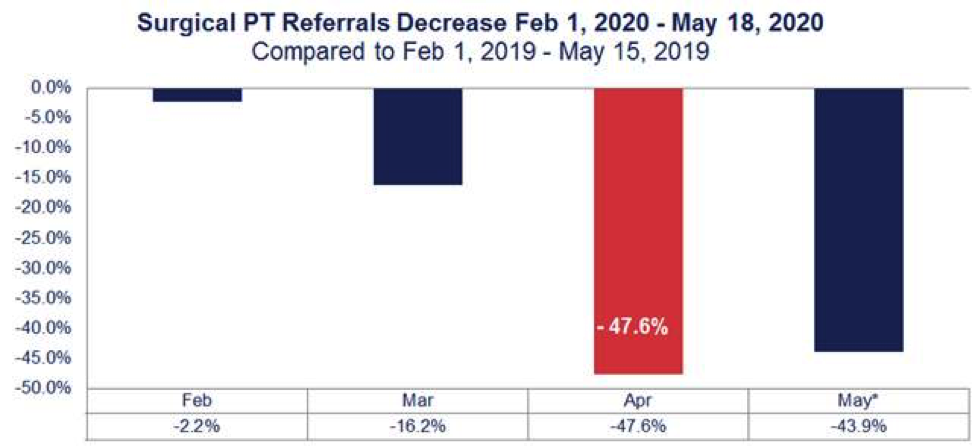
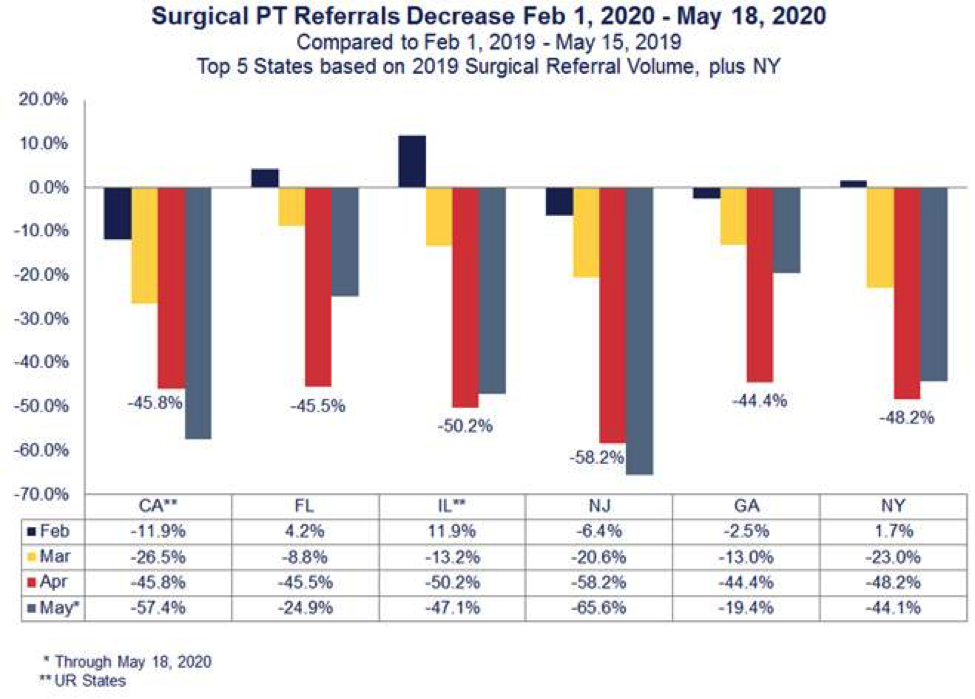
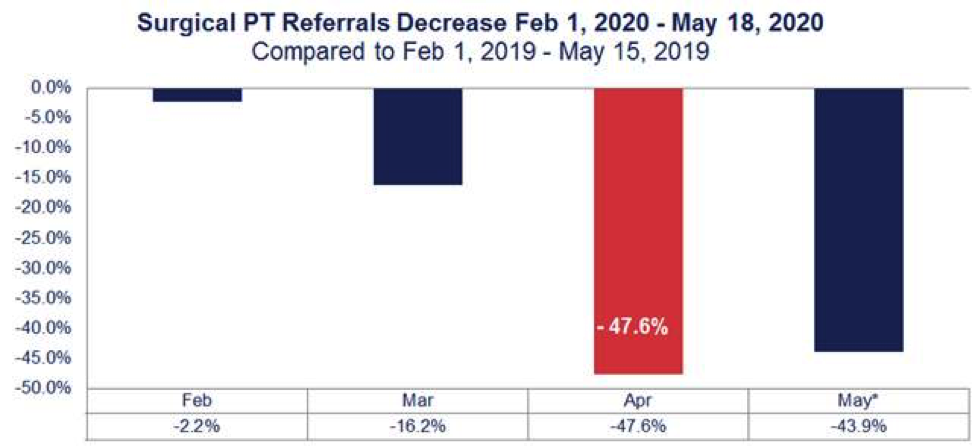
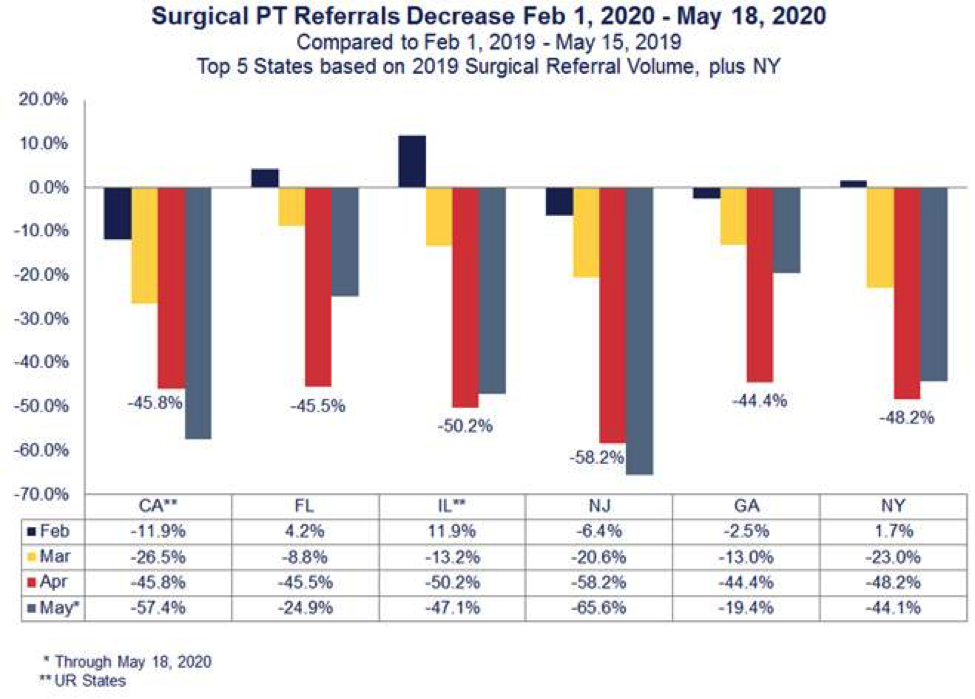
MedRisk’s post-surgical PT referrals were down 47.6% percent nationwide in April when comparing data to a year prior (Figure 1). And it some states, like New Jersey, that decrease was even more significant at 58.2% (Figure 2). However, in late April, more than 30 states gave the green light to hospitals and surgical centers to resume surgeries. MedRisk expects that the industry will begin seeing a surge in physical therapy as more injured workers get back on schedule over the next few months – but perhaps with some differences from before the pandemic.
The NCCI predicts that the deferral of hospital treatments and physical therapy will mean longer claim duration, which can equate to higher indemnity payments and likely more overall medical expenditure. This, combined with the fact that claimants cannot return to work after medical treatment if work is furloughed, may lead to higher severity for active workers’ comp claims.
In addition, a break or delay in treatment can add inherent complexities to treatment. During stay-at-home orders, some patients have lost the physical strength and tone surgery requires. Therefore, claims representatives can expect to receive prescriptions for pre-operative conditioning; providers and claims professionals may also see psychosocial barriers to recovery such as anxiety related to COVID-19, catastrophic thinking, perceived injustice and fears/avoidance as injured workers finally begin treatment.
Looking to the Future
As employers, payers and providers prepare for these impacts, MedRisk’s existing programs provide the infrastructure needed to effectively guide injured workers through these hurdles. MedRisk’s extensive national network remains poised to manage the increase in visits that may be needed to get this subset of injured workers back on their feet.
Now more than ever, it is important to have a managed care partner that goes beyond scheduling and basic visit management. Our pre-therapy patient consultations are designed to detect psychological barriers to recovery and to educate patients about the rehabilitation process after delays in treatment. This patient-centered approach, together with our evidence-based guidelines, allows payers and providers to make clinically-informed decisions that support when, how and where to start rehabilitation – even in the most extraordinary of circumstances.