Nov 4, 2020 | Insights
Should symptoms-based physical treatment remain the go-to approach for treating chronic LBP?
Over the last decade, cognitive interventions have become the subject of dialogue and research regarding the treatment of chronic low back pain (LBP). Studies have shown that cognitive interventions, such as those that address perceptions of pain, demonstrate similar rates of effectiveness in self-reported disability and sick leave when compared to traditional treatments. These findings were tested further in the first study to compare a cognitive education method based on a non-injury model with that of more traditional symptom-based physical training for chronic LBP.
In BMC Musculoskeletal Disorders, Sorensen et al shared the framework for this study, which compared (1) an educational approach designed to improve confidence in the robustness of the spine and (2) symptom-based physical training treatment. Primary outcomes were back pain and activity limitation, and secondary outcomes were attitudes regarding LBP, physical activity levels, work ability, quality of life, sick leave, as well as various other healthcare treatments.
The study found that, despite having fewer treatment sessions, cognitive, education intervention for chronic LBP resulted in at least equivalent outcomes as a symptom-based physical training method. These findings support MedRisk’s commitment to providing consultations to injured workers in advance of treatment to educate patients on the importance of physical therapy, describe what to expect, and address any perceived barriers to recovery.
Sorensen, P.H., Bendix, T., Manniche, C. et al. An educational approach based on a non-injury model compared with individual symptom-based physical training in chronic LBP. A pragmatic, randomised trial with a one-year follow-up. BMC Musculoskelet Disord 11, 212 (2010). https://doi.org/10.1186/1471-2474-11-212

Oct 29, 2020 | Insights
CompTalk is a new session format for the National Workers’ Compensation and Disability Conference – National Comp
Initially thought to solve access issues for workers’ compensation patients in rural areas or working shifts, telerehabilitation ended up being used more for convenience since MedRisk introduced it in 2017.
While many payers appreciated the patient satisfaction it produced, others were slow to adopt.
COVID-19 changed all that. Some jurisdictions closed physical therapy clinics for weeks. Decreased patient volume caused other clinics to reduce their hours or close temporarily. And some patients chose not to start or continue in-clinic treatment during the pandemic.
Suddenly access was the issue, and without telerehab, some injured workers would receive no physical therapy.
MedRisk’s Vice President of Clinical Services and Provider Relations Brian Peers, DPT, MBA discusses this transition and its lessons during “Telerehab During a Time of Crisis,” a fast-paced CompTalk available on demand at https://wcconference.com/telerehab-in-times-of-crises/ .
Dr. Peers recalls embracing the sudden change, pivoting patients toward telerehab, and shares lessons learned during the TED-Talk-like presentation. “We found many conditions previously recommended for in-clinic care, could be treated just as successfully via telerehab,” he said.
He also discusses the future of telehealth and suggests takeaways for workers’ compensation professionals.
Launched this year by the National Workers’ Compensation and Disability Conference – National Comp, CompTalks are a new series of short videos, designed to educate, enlighten, and inspire meaningful conversations. MedRisk is also a Gold Sponsor of the 2020 National Comp conference, which went virtual this year, starting with a free, one-day telecast on October 21, followed by digital educational sessions scheduled two to three times a month until the 2021 live conference in the fall.
About MedRisk
Based in King of Prussia, Pennsylvania, MedRisk is the largest managed care organization dedicated to the physical rehabilitation of injured workers. Clinically driven since its inception, the company has an International Scientific Advisory Board that developed and maintains physical medicine-specific, evidence-based guidelines for workers’ compensation. MedRisk, which has successfully completed a SSAE 18 SOC Type 1 and 2 examinations, ensures high quality care and delivers outstanding customer service. For more information, visit www.medrisknet.com or call 800-225-9675.
Sep 15, 2020 | Insights
A recent publication explores the essential role of physical therapists in helping patients develop self-management strategies to combat musculoskeletal pain.
In a recent article published in the Journal of Orthopaedic & Sports Physical Therapy, Hutting et al discuss the issue of persistent musculoskeletal pain, including low back pain, in a global context and the dialogue surrounding effective treatment approaches.
The authors advocate for a “person-centered approach,” with physical therapists encouraging more active participation from the patient. They contend that treatment focused on self-management gives patients the skills and knowledge to actively manage their pain.
The self-management approach means educating patients on the biomechanical and psychosocial aspects of their conditions and involving them in decision making. The goal is to equip them to self-regulate their pain well after PT sessions end.
Recommendations include the formation of a strong patient-provider relationship with self-management support tailored to the patient’s unique needs. There is a focus on behavior change, an active lifestyle, and a positive attitude.
MedRisk is in alignment with these recommendations and helps facilitate a person-centered approach for patients through consultation with an on-staff PT in advance of treatment and in cases of interrupted recovery. Self-management is also a primary goal for treatment in the MedRisk Telerehabilitation Program.
Hutting, N., Johnston, V., Staal, J. B., & Heerkens, Y. F. (2019). Promoting the use of self-management strategies for people with persistent musculoskeletal disorders: the role of physical therapists. journal of orthopaedic & sports physical therapy, 49(4), 212-215.

Sep 14, 2020 | Insights
Research has shown broadly that early PT can improve outcomes and reduce utilization of other medical services. WCRI’s new study examines how this plays out in workers’ comp cases.
Physical therapy (PT) has become a widely accepted and critical conservative care recommendation for low back pain (LBP) in the last decade, reducing the need for other, more invasive procedures and opioid prescriptions. As such, the timing of PT has become the subject of a number of studies which have proven early is better. Early treatment improves outcomes and reduces the utilization of other medical services.
Building on this research, the highly respected Workers’ Compensation Research Institute (WCRI) has conducted the most comprehensive study addressing PT timing focused on workers’ compensation patients. One of the researchers, Dr. Kathryn Mueller, is a member of MedRisk’s International Scientific Advisory Board.
Here are the study details, key findings and critical takeaways for the workers’ comp industry.
Study Details
The study looked at how different timing of PT may impact:
- The utilization of MRIs, opioid prescriptions, pain management injections, and lumbar surgeries
- Total medical costs per claim (not just PT)
- How many weeks of temporary disability benefits are used per claim
Vague terms like “early” and “late” have been interpreted any number of ways in existing research. In this study, WCRI examined the outcomes of five PT-timing groups (within 3 days, 4-7 days, 8-14, 15-30 and more than 30-days post injury) and defined “late PT” as more than 14 days of injury.
Key Findings
Patients who received early PT (within three days of injury) were:
- 46% less likely to receive opioid prescriptions
- 47% less likely to receive an MRI
- 29% less likely to receive pain management injections
- Less likely to involve an attorney in the claim (14% average involvement) than those who received late PT
Patients who received late PT (more than 30 days after injury):
- Were on temporary disability that lasted 58% longer
- Were 89% more likely to have low back surgery
- Had an average attorney involvement of 27%
It is important to note that even “late” PT can still improve outcomes over no PT at all. Across all claimants, and regardless of timing, fewer than 5% had back surgery.
Critical Takeaways
This cornerstone study clearly supports the value of including PT as a first-line treatment option and removing barriers to early PT.
While the researchers say further study is needed, the findings that early PT is “likely to be beneficially associated with a lower utilization of medical services, lower overall medical costs, and shorter temporary disability” is critical validation of the importance of physical medicine in treating injured workers.
So what can make a positive impact on workers’ comp claims? Experience shows that rapid scheduling, patient advocacy, clinical guidance that supports conservative care first, integrated technology, and a management program that connects patients with the right PT quickly have a significant impact on outcomes and cost.

Aug 13, 2020 | Insights
As companies establish a “new normal” for their operations, will injured worker treatment also get back on track?
As social distancing guidelines are lifted and communities around the country begin to reopen, employers are readying their workplaces for employees to return to work. However, there is one faction of the workforce for which the wait has felt particularly long, and that’s workers who have been hurt on the job before COVID-19.
In March, while the country hunkered down to “flatten the curve” of coronavirus cases in hospitals, healthcare systems braced for a potential influx of COVID-19 patients by suspending non-emergency surgical procedures, as recommended by the American College of Surgeons. As a result, researchers have estimated that 244,400 orthopedic surgeries were canceled each week during the 12-week peak disruption period in North America alone, including back surgeries, hip and knee replacements and other operations for those hurt on the job.
For many injured workers, treatment – both surgery and post-surgical physical therapy – has been put on pause. What effects has this had on physical medicine patients and providers in the workers’ comp industry, and what can we expect as the healthcare system rebounds? Let’s take a closer look.
Postponement of Elective Surgeries and Its Impact on PT
How much backlog will the healthcare system be facing as hospital operations resume?
According to an analysis from Strata Decision Technology, over a two-week period in March and April 2020, patient encounters in a hospital setting fell 54.5% when comparing it to the same period a year prior. And no specialty was immune – this trend was seen across all services lines, in every region. Primary knee replacements fell 99%, lumbar/thoracic spinal fusions declined 81% and primary hip replacement procedures fell 79%. Researchers predict that if countries increase their normal surgical volume by 20 percent post-pandemic, it would take a median 45 weeks to clear the backlog of operations.
The CDC categorized physical therapy as an essential service during the pandemic, and many patients were able to continue treatment either in-person or via telerehabilitation. However, the cancelation of elective surgeries – and with it, expected post-surgical physical therapy treatment – and patient concerns over possible viral transmission in a clinic setting had a negative impact on PT numbers nationwide. These data indicate that both orthopedists and physical therapists can expect to be managing the backlog of postponed procedures and treatment over the next year.
Effects on Workers’ Comp
PT numbers have followed a similar trend in workers’ comp. In respect to new claims, the National Council on Compensation Insurance (NCCI) expects that due to economic and employment trends, injury frequency is likely to continue its decline in most sectors, with the exception of warehousing, where there has been a hiring surge.
Pre-COVID-19, the workers’ comp industry was seeing injury rates and frequency decline overall. MedRisk data also showed a five-year trend in declining surgical cases, from 23.5% in 2015 to 17.3% in 2019; however, the number of lost time claims with physical medicine involvement continued to increase. Will the PT and conservative care movement continue in workers’ comp moving forward?
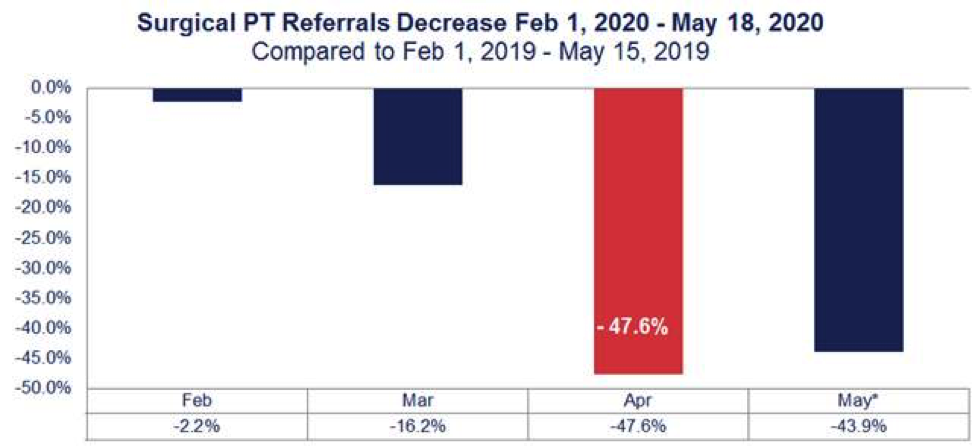
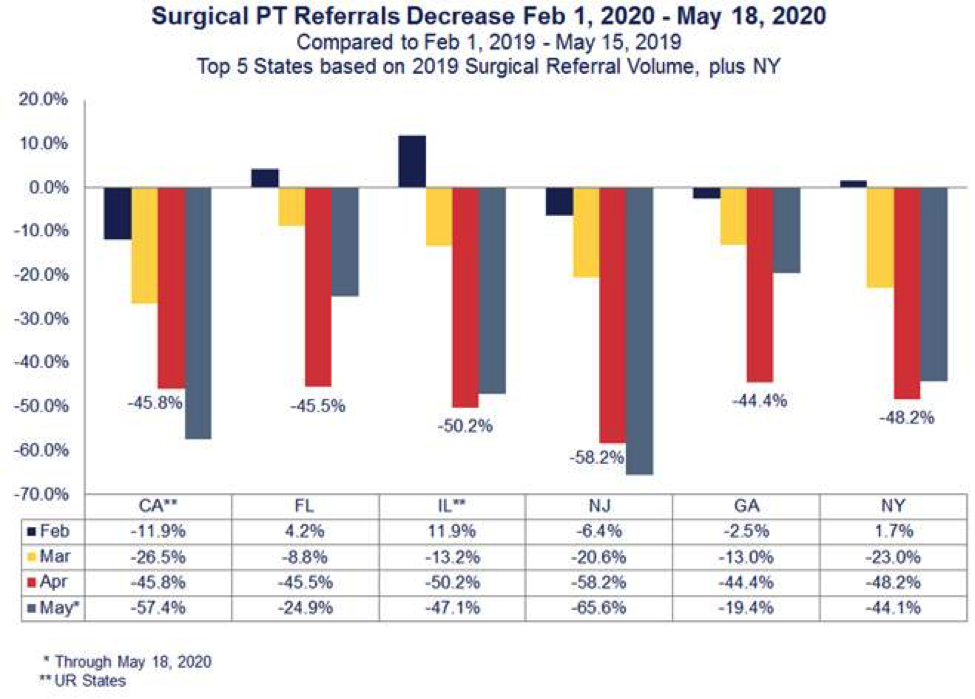
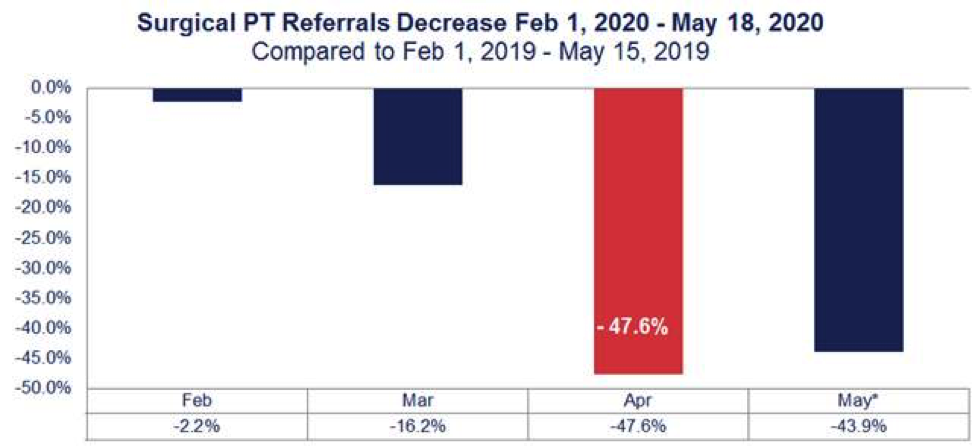
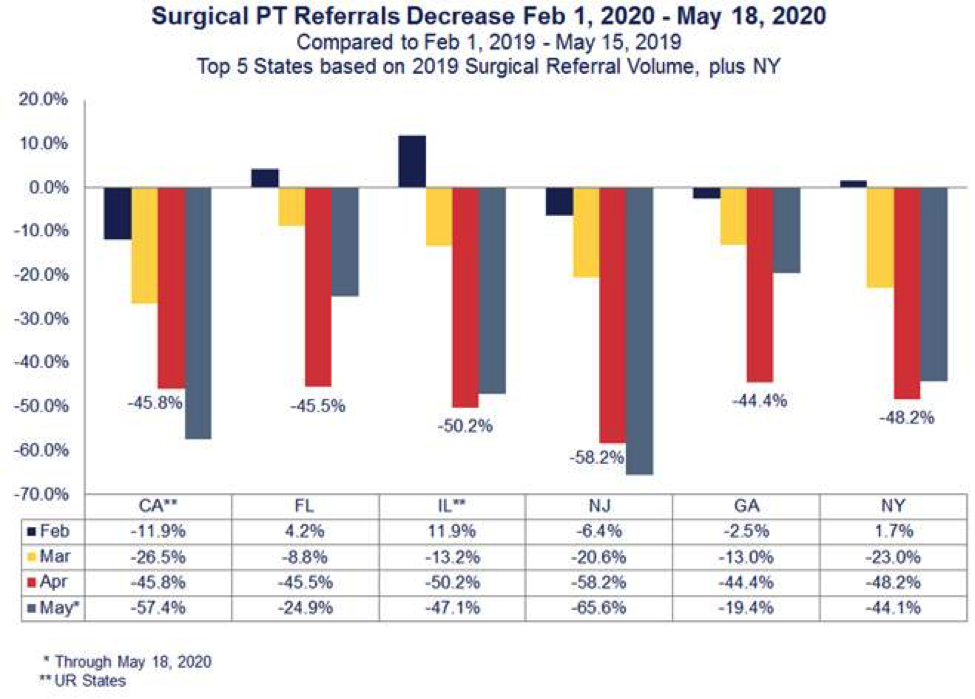
MedRisk’s post-surgical PT referrals were down 47.6% percent nationwide in April when comparing data to a year prior (Figure 1). And it some states, like New Jersey, that decrease was even more significant at 58.2% (Figure 2). However, in late April, more than 30 states gave the green light to hospitals and surgical centers to resume surgeries. MedRisk expects that the industry will begin seeing a surge in physical therapy as more injured workers get back on schedule over the next few months – but perhaps with some differences from before the pandemic.
The NCCI predicts that the deferral of hospital treatments and physical therapy will mean longer claim duration, which can equate to higher indemnity payments and likely more overall medical expenditure. This, combined with the fact that claimants cannot return to work after medical treatment if work is furloughed, may lead to higher severity for active workers’ comp claims.
In addition, a break or delay in treatment can add inherent complexities to treatment. During stay-at-home orders, some patients have lost the physical strength and tone surgery requires. Therefore, claims representatives can expect to receive prescriptions for pre-operative conditioning; providers and claims professionals may also see psychosocial barriers to recovery such as anxiety related to COVID-19, catastrophic thinking, perceived injustice and fears/avoidance as injured workers finally begin treatment.
Looking to the Future
As employers, payers and providers prepare for these impacts, MedRisk’s existing programs provide the infrastructure needed to effectively guide injured workers through these hurdles. MedRisk’s extensive national network remains poised to manage the increase in visits that may be needed to get this subset of injured workers back on their feet.
Now more than ever, it is important to have a managed care partner that goes beyond scheduling and basic visit management. Our pre-therapy patient consultations are designed to detect psychological barriers to recovery and to educate patients about the rehabilitation process after delays in treatment. This patient-centered approach, together with our evidence-based guidelines, allows payers and providers to make clinically-informed decisions that support when, how and where to start rehabilitation – even in the most extraordinary of circumstances.

Feb 5, 2020 | Insights
Dr. Steven George explains how PTs can treat those who have had musculoskeletal pain during COVID-19
Chronic pain is not a new problem in the United States. It is one of the most common reasons for seeking medical care and has been linked to anxiety and depression, poor health and reduced quality of life and, as seen in the news, a dependence on opioid prescriptions.
However, this is the first time in recent history that those managing pain are doing so through a pandemic. As mounting research points to the effectiveness of conservative care, physical therapy has asserted a central role in both preventing and managing long-term musculoskeletal pain. How can physical therapists best support patients during a time when postponed treatment puts musculoskeletal patients at a higher risk of delayed recovery and chronic pain?
To learn more, we sat down with MedRisk International Scientific Advisory Board (ISAB) member Steven Z. George, PT, PhD, FAPTA, from Duke University’s School of Medicine. He is the Laszlo Ormandy Distinguished Professor in Orthopaedic Surgery and also serves as Director of Musculoskeletal and Surgical Sciences for the Duke Clinical Research Institute and Vice Chair of Research for the Department of Orthopaedic Surgery.
The Psychosocial Factors of Pain
Helping injured workers manage musculoskeletal pain is a primary focus for physical therapists, but according to Dr. George, effective treatment often encompasses more than addressing physical symptoms. An emerging topic of PT research is how beliefs and emotions impact the pain experience.
Especially in the case of an on-the-job injury, psychosocial factors, which include pain-related fears, perceived injustice, and fear of reinjury, can prevent a patient from being active in their rehabilitation. This can then significantly impact recovery. According to Dr. George, pain catastrophizing (another psychosocial factor), which is associated with pessimism and helplessness, can lead to poor outcomes in musculoskeletal injury. Depression and anxiety, whether specific to the injury or a general trait, can also affect potential for recovery.
“We have 25 years of literature where researchers were looking for one particular factor that posed the most risk to recovery – a ‘ring to the rule them all,’” he added. “But what we have found is there’s not just one, and it’s not even just about the number of factors that are elevated. They compound. So, this needs to be considered as a cumulative risk model.”
This research is supported by the use of screening tools, such as the STarT Back Screening Tool, the Optimal Screening for Prediction of Referral and Outcome tools, or the Örebro Musculoskeletal Pain Questionnaire (ÖMPQ) MedRisk uses to assess for psychosocial factors, in a rehabilitation patient.
It is not uncommon for patients to exhibit 1 or 2 psychosocial factors, but when this number increases, there is a higher risk of delayed recovery. Although it’s too early to say, it’s reasonable to expect to see more of these boxes being checked by workers’ comp patients in 2020 and 2021.
“Everyone talks about the second wave of COVID-19, but we are also concerned about the second wave of pain management. As treatment resumes, it may be harder to change negative beliefs and fears related to work injury. And when you think about catastrophizing, this pandemic is also a ‘hand that’s been dealt’ to us all,” Dr. George said.
As hospitals have postponed surgeries and PT treatment has been delayed, many patients have not had the same level of access to nonpharmacologic pain management options, such as PT, during the pandemic. These factors, combined with the psychological impact of such a profound event, will likely equate to a different experience of pain – and likewise, a different course of treatment – for these patients moving forward.
Psychologically Informed Physical Therapy
How should PTs adapt their approach to delivering treatment as the country continues to fight coronavirus? The answer includes implementing safety precautions, like masks and disinfecting, to mitigate the spread of the virus – and more. Many clinicians are embracing the principles of psychologically informed practice, as it bridges the gap between standard PT practice, based on biomedical tenets, and a more cognitive-behavioral approach, derived from principles of mental health treatment. (Click here to learn more about related research from MedRisk ISAB member Dr. Chris Main.) The main goal is to identify psychosocial signs, or “yellow flags,” that may affect treatment outcomes.
Using screening tools like those mentioned above, PTs then adapt standard treatments to incorporate, for example, deep breathing exercises, mental imagery and progressive muscle relaxation, to ease the pain associated distress and improve outcomes.
One way to prompt a discussion about the patient’s pain experience is through motivational interviewing, a counseling technique that helps patients resolve ambivalent feelings and insecurities and find internal motivations to change their behavior. In taking this personalized approach, PTs can also open the door to exploring the relationship between fear and movement. A behavioral approach to exercise is one of the hallmarks of psychologically informed practice.
“If a patient stops an exercise and says it hurts, the PT needs to understand whether they are stopping because they are experiencing injury or because they are experiencing pain,” Dr. George said. “Not all pain is bad; successful rehab involves working through some of the pain. That’s how the system adapts.”
Psychologically informed physical therapy encourages PTs to incorporate “gentle pushback” to lead patients to a place where they see the value of stretching themselves to do 10 minutes of exercise while bearing some discomfort, rather than stopping at 5. This approach is all predicated on the assumption that the exercises being prescribed by the PT are not harmful.
These types of conversations during therapy also encourage patients to take an active part in their recovery, which Dr. George believes is particularly important to treating today’s PT patients. Self-management is a part of all treatment guidelines, but as the use of telerehabilitation rises, PTs must reassure patients that their participation is part of a team-based approach.
“You don’t want the patient to take it as ‘It’s all on you. It’s more ‘We are going to work on finding techniques that work for you, together,” he said.
Conclusion
During these uncertain times, patients may start treatment later than planned or in a different method than expected (i.e., telerehabilitation). However, PT remains one of the most valuable methods for preventing or managing long-term musculoskeletal pain.
Conservative care, particularly immediately after injury, has been shown to be effective and to have a protective effect against opioid use, but even patients who may have been given a short-term pharmacologic treatment can see beneficial effects through physical therapy. The entire care team, including the patient, needs to be involved in developing a long-term treatment plan of which physical therapy may be a part.
No matter the patient’s circumstances, clinicians should assume that the pandemic has had an impact on their recovery and, like so many aspects of pandemic life, treatment will require adaption to be most effective.
“Whether the patient’s injury is physically affected by COVID-19 or not, we should be sensitive to just how stressful it must have been to be in pain during this time,” Dr. George said. “Let the patient state that simple fact without the PT feeling like it needs to be fixed. Be open to recognizing [the pandemic] as something that has made this recovery much, much harder and allow that to be a part of treatment.”